Dr. Quinn named as Presidential Fellow at ETSU
Dr. Megan Quinn
Associate Professor in Epidemiology
JOHNSON CITY (April 20, 202) – East Tennessee State University President Brian Noland has named Dr. Nicholas Hagemeier, Dr. Jodi Polaha and Dr. Megan Quinn as Presidential Fellows for the fall 2020 semester.
As fellows, the three faculty members will develop and execute a project that is aligned with one of the university’s major initiatives in teaching, learning and service. The fellows will work closely with President Noland, his leadership team and ETSU Center for Teaching Excellence staff.
Hagemeier has been at ETSU since 2011. He is vice chair and associate professor of Pharmacy Practice and director of Student Professional Development at Bill Gatton College of Pharmacy.He also serves as director of ETSU’s Pharmacy Practice Research Fellowship. He earned his Pharm.D., M.S., andPh.D. degrees fromPurdue University. He was awarded National Institutes of Health funding to conduct research on the role of pharmacists in preventing opioid-related morbidity and mortality and has presented opioid- and wellbeing-related research nationally. He was appointed to the U.S. Health and Human Services Pain Management Best Practices Interagency Task Force in 2018.
Hagemeier’s project will focus on meeting wellbeing-related initiatives in ETSU’s Strategic Plan.
Polaha is a clinical psychologist and associate professor in the Department of Family Medicine at ETSU’s Quillen College of Medicine. She has over 20 years of experience integrating behavioral health into primary care in clinical, teaching, research, and policy roles and currently serves as assistant director of Interprofessional Education.
She has a strong interest in increasing practice-based research and serves as a co-editor for the journal Family, Systems, & Health. Polaha has a long history of community service and was elected to serve on the Washington County Board of Commissioners in 2018.
Polaha’s project will focus on ETSU’s role in regional workforce development.
Quinn is an associate professor of epidemiology in the Department of Biostatistics and Epidemiology in the College of Public Health. She teaches courses in infectious disease epidemiology, field epidemiology and global health. She earned her B.A. in psychology from Wesleyan College, a M.Sc. in public health research from University of Edinburgh College of Medicine and Veterinary Medicine, and a Dr.PH in epidemiology from ETSU.
She has taught at ETSU since 2012. In 2016, she earned the ETSU Distinguished Faculty Award in Service. Her research is primarily focused on adverse childhood experiences (ACEs) and their role in health risk behaviors and outcomes.
Quinn’s project will focus on understanding the current campus climate as it relates to ACEs-informed practices and work to identify opportunities to promote ACEs awareness.

Dr. Maisonet Elected to International Society
Dr. Mildred Maisonet
Assistant Professor in Epidemiology
Dr. Mildred Maisonet, Assistant Professor in East Tennessee State University College
of Public Health’s Department of Biostatistics and Epidemiology, has been elected
as a Councilor for North America for The International Society for Environmental Epidemiology.
The International Society for Environmental Epidemiology to impact research, training, and policy worldwide. With a membership of over 1000 scientists from 61 countries, the society provides a forum for the debate of issues unique to the study of health and the environment. To society’s goal is to foster epidemiological studies on the effects of environmental exposures in people, stimulate communication between health professionals, promote methodological advances, and strengthen environmental health policy.
“Throughout my career, the ISEE meetings and other activities have provided an important space for professional growth and scientific engagement,” stated Dr. Maisonet. “The benefits I have reaped from my membership would not have occurred without the hard work of the many dedicated ISEE members who have held office before me. Being elected as councilor has given me the opportunity to serve back.”
Dr. Maisonet will be serving as a Councilor for the period 2020-2022.
Doctoral Student Co-Authors Article on Spina Bifida
Ogbebor Omoike
Doctor of Public Health student, Epidemiology
Ogbebor Omoike, student in East Tennessee State University College of Public Health’s doctoral program, is co-author of an article in the Journal of Pediatric Rehabilitation Medicine. The article, “The reliability and validity of a newly developed spina bifida-specific transition readiness assessment questionnaire: Transition readiness assessment questionnaire-supplement (TRAQ-SB)” reports preliminary evidence to support a new condition-specific measure of transition readiness that is theoretically grounded in the Stages of Changes framework.
Lead author of the article is Kiana Johnson of the Quillen College of Medicine. Additional co-authors include Brandon Rocque and Katherine Barnes of the University of Alabama and David Wood of the Quillen College of Medicine.
Spina bifida is a neural tube defect that is usually apparent at birth and occurs when the backbone that protects the spinal cord does not fully close during development. The neural tube is the structure in a developing embryo that eventually becomes the baby's brain, spinal cord and the tissues that enclose them. Spina bifida can cause physical and intellectual disabilities that range from mild to severe mostly based on the size and location of the opening in the spine and the nerves affected.
The Transition Readiness Assessment Questionnaire-Spina Bifida (TRAQ-SB) supplement is a newly developed tool used to measure independence and skill acquisition related to spina bifida. Similar to the Transition Readiness Assessment Questionnaire (TRAQ), the TRAQ-SB uses a 5-point Likert response set.
Working with a multi-disciplinary team with expertise in the care of children with spina bifida, the authors developed twelve items pertaining to main aspects of SB self-management. The items were reviewed and revised through several iterations by the team and patients. The items were then fielded at a spina bifida Specialty Clinic, where 90 consecutive patients between the ages of 12 and 25 were administered the 20-item TRAQ and a 12-item TRAQ-SB questionnaire.
Results of the researchers’ analyses indicated that the TRAQ-SB demonstrated good internal reliability and criterion validity as evidenced by strong correlation with age and the validated TRAQ measure. The TRAQ-SB tool can be useful to incorporate transition readiness assessment and self-management training into routine care for adolescents with spina bifida.

Dr. Maisonet and Student Featured in Illuminated Magazine
Dr. Mildred Maisonet and Denise Chavez
Assistant Professor and MPH Student in Epidemiology
Dr. Mildred Maisonet and Denise Chavez Reyes were featured in Illuminated Magazine
for their work with phthalate exposure.

College Publishes on Obesity Factors in sub-Saharan Africa
Dr. Ifeoma Ozodiegwu
Doctor of Public Health alumna, Epidemiology
Students, alumni, and faculty from East Tennessee State University’s College of Public Health have published on sociocultural factors that predispose women and girls in sub-Saharan Africa to become overweight or obese. The article, "A qualitative research synthesis of contextual factors contributing to female overweight and obesity over the life course in sub-Saharan Africa" appeared in PLOS ONE.
Dr. Ifeoma Ozodiegwu, alumna of the college’s doctor of public health program, is lead author of the article. Drs. Mary Ann Littleton, Megan Quinn, and Hadii Mamudu, college faculty, are co-authors along with current doctoral students Christian Nwabueze and Oluwaseun Famojuro. Dr. Richard Wallace of the Quillen College of Medicine also co-authored the article.
Understanding the factors that cause women in sub-Saharan Africa to become obese is one of the global voluntary targets outlined in the World Health Organization Global Action Plan for the Prevention and Control of Non-communicable Diseases. One of the overarching principles of the plan is the recognition that a life-course approach to the prevention and control of disease is crucial. Adopting a life-course approach permits the identification of potential adiposity risk factors and prevention needs at multiple life stages.
In this report, the authors aggregate research literature on contextual factors that potentially predispose adult women and adolescent girls to overweight and obesity. An exhaustive search was conducted in PubMed to identify journal articles and dissertations related to the study aims. After the removal of duplicates and any studies conducted prior to 2000, a total of 446 records remained. After critical appraisal, a total of 17 studies were included for this report.
Three major themes: body size and shape ideals, barriers to healthy food choices, and barriers to engaging in physical activity were identified from the thematic analysis. In the description of these themes, sub-themes within each overarching theme were presented for both adult women and adolescent girls.
From their analysis, the researchers concluded that sociocultural, institutional and peer-related factors were powerful forces shaping body size preferences, food choices and participation in physical activity. They also found a number of adverse effects from the institutionalization of body size and shape ideals including weight-related victimization among adolescents and stigmatization of thinness due to a perceived link with HIV. The authors call for further research to translate these findings into community-based interventions that can reduce overweight and obesity in sub-Saharan Africa.
Doctoral Student Presents on Smoking and Homocysteine Levels
Ogbebor Omoike,
Doctor of Public Health student, Epidemiology
Ogbebor Omoike, student in East Tennessee State University College of Public Health’s doctoral program, presented at the American College of Epidemiology’s Annual Meeting in Pasadena, California in September 2019. The presentation, “Association between smoking status and homocysteine levels and possible effect modification by cholesterol and estradiol” discusses the amino acid homocysteine and its possible relationship with whether or not a person smokes.
Environmental and dietary exposures alter the levels of homocysteine in the human body; however, little is known about the association of smoking status with homocysteine levels. This study aimed to examine the association of smoking status with homocysteine levels and to determine whether the association is modified by estradiol, a female hormone, or cholesterol, a type of lipid.
Data were obtained from National Health and Nutrition Examination Survey 2003-2004 with analysis done in 2018 on 4,580 adults aged 20 years and older. A current smoker defined as a person who smoked at least 100 cigarettes in his/her lifetime and at least once in the last month; a former smoker is one who had smoked less than 100 cigarettes and had quit smoking at the time of the interview; a “never smoker” is an adult who never smoked cigarettes in their lifetime or less than 100 cigarettes in his/her lifetime.
After adjusting for age, sex, ethnicity, education, and income level, homocysteine levels did differ by smoking status. The addition of estradiol as an interaction term in adjusted models was associated with a 16.6% increase in homocysteine levels when compared to models without the interaction term. Estradiol but not cholesterol did moderate the association between smoking status and homocysteine levels.
The study concluded that homocysteine levels did differ across smoking status after adjusting for confounders. Estradiol did moderate the relationship between homocysteine and smoking status. This suggests that smoking may have long-term negative effects on homocysteine levels with estradiol exacerbating this relationship particularly in current smokers, hence, the importance of programs to prevent smoking initiation and close monitoring of estradiol levels in current smokers who are also on hormone replacements or who are obese.

College of Public Health Alumni Publish on Uninsurance
Dr. Ifeoma Ozodiegwu and Dr. Shaoqing Gong
Doctor of Public Health alumni, Epidemiology
Dr. Ifeoma Ozodiegwu and Dr. Shaoqing Gong, alumni of East Tennessee State University College of Public Health’s Doctor of Public Health program, have published an article in Quantitative Finance and Economics. The article, “Multivariate analyses of social-behavioral factors with health insurance coverage among Asian Americans in California,” estimates the prevalence of health insurance and variables associated with individuals who are not insured.
Faculty from Hunan University, West Virginia University and the East Tennessee State University College of Business and Technology are co-authors.
Studies have shown racial differences in uninsurance rate among adults in the United States. Few studies have focused on social-behavioral factors with uninsurance rate among Asian Americans. This study aimed to estimate the weighted prevalence of uninsurance among Asian Americans of Chinese, Filipinos, Japanese, Koreans, and Vietnamese ancestry, and compare it with Whites, African Americans and Latinos. A second objective of the study was to evaluate the associations of smoking, citizenship, and socioeconomic status with uninsurance.
A total of 24,136 adults (aged 18–64) including 2,060 Asian Americans were selected from the combined 2013–2014 California Health Interview Survey. Among Asians, compared to Koreans, being Filipinos or Vietnamese was associated with lower odds of being uninsured; meanwhile being male, non-citizen, lower education, and higher poverty were significantly associated with increased odds of uninsurance. Elder age groups and current smoking were significantly associated with increased odds of uninsurance in bivariate analysis; however, such associations disappeared after adjusting for other factors.
There are differences in prevalence of uninsurance between Asians and Whites, and among Asian subgroups. However, compared to previous estimates, there appears to be a downtrend in uninsurance estimates for Koreans and Vietnamese. Being male, lower education, higher poverty, non-citizen, and current smoking were positively significantly associated with uninsurance. These findings can help design better interventions to reduce racial and ethnic disparities in uninsurance, especially for Asian Americans. To date, there is very limited research examining uninsurance among Asian Americans. Therefore, it is important to identify the factors propelling the uninsurance rate in this population, in order to effectively reduce the number of uninsured individuals.

Dr. Ying Liu Participates in OHSU Orthodontics Study
Dr. Ying Liu
Associate Professor, Biostatistics
Dr. Ying Liu, Assistant Professor in East Tennessee State University College of Public Health’s Department of Biostatistics and Epidemiology, is part of a study funded by the National Institutes of Health to research how mechanobehavior affects of outcomes of orthopedic appliances in brachyfacial and dolichofacial children.
Dr. Laura Iwasaki, Chair of Oregon Health & Science University Orthodontics, is principal investigator of the study. Co-investigators include Dr. Liu as well as Drs. Michelle Kim, Hongzeng Liu, and Jeff Nickel of OHSU, and Dr. Luigi Gallo of the University of Zurich.
Each year, across the United States, treatment of malocclusions costs more than $9.5 billion, and represents the third largest category of dental procedures for people under 20 years of age. Approximately one third of malocclusions involve treatment of skeletal discrepancies due to mandibular retrognathism. The annual failure rates of mandibular growth enhancement therapies results in direct costs of greater than $700 million dollars. Furthermore, poor results may require the surgical management of the malocclusion, which adds morbidity risk and considerably more financial costs.
The focus of the study is to identify how TMJ intracapsular mechanics, and day- and night-time muscle activities differentially affects outcomes of orthopedic appliances in diagnostic subgroups of growing children. The long-term goal of the research is to identifying practical ways to improve outcomes and reduce the financial burdens of unsuccessful therapies.

College of Public Health Alumnus Selected for CDC Fellowship
Dr. Daniel Owusu
Alumnus, Epidemiology
Daniel Owusu, alumnus of East Tennessee State University College of Public Health’s doctor of public health program, has been accepted to join the 2019 class of the Epidemic Intelligence Service (EIS) of the Centers for Disease Control and Prevention (CDC). CDC describes the EIS as a “2 year post-doctoral training program for health professionals interested in practice of applied epidemiology”. EIS is a “long-standing, globally-recognized fellowship program, renowned for its investigative and emergency response efforts.”
He will work with the Epidemiology and Prevention Branch in the Influenza Division at the National Center for Immunization and Respiratory Diseases located in Atlanta.
“The EIS is one of the most prestigious fellowship available, and one of the most important, for young professionals with expertise in Epidemiology. These are the celebrated “Disease Detectives” who play such an important role in protecting the country, and the world, from a wide variety of diseases and health conditions,” said. Dr. Randy Wykoff.
During his doctoral program in ETSU, Dr. Owusu undertook an internship with the World Health Organization African Region office to work on tobacco and noncommunicable disease control in order to experience public health practice in low-resource settings. He completed his dissertation on tobacco smoking cessation in low-and-middle income countries. Since graduating from ETSU, Dr. Owusu has been researching on how to communicate about novel and alternative tobacco products, risk perception, and epidemiology of novel and alternative tobacco product use as a Postdoctoral Research Associate at Georgia State University. In addition, he is a key collaborator of the Tobacco Policy Research Group (TPRG) in ETSU, and a member of the Sub-Sahara Tobacco Policy Research Group (SATRG). He has authored or co-authored 27 peer-reviewed journal publications that focused on tobacco, genetics, cancer and diabetes.
“It is an exciting moment for me to join the EIS class of 2019 and I look forward to greater opportunities during and beyond the EIS fellowship. I see my acceptance into the EIS class as a significant step that draws me closer to my dream of becoming a leader in public health,” said Dr. Owusu. “It was this dream that influenced my decision to pursue the DrPH degree program in the ETSU College of Public Health.”
Dr. Wykoff added “Since 2011, there have been 18 students with DrPH degrees admitted into the EIS program. Even though there are over 75 DrPH programs in the country, we are honored that four of these 18 EIS Officers are graduates of ETSU.”
“The great exposures during my doctoral training at ETSU, including a global public health experience, and the invaluable supports from the faculty, staff, and alumni of the college have immensely contributed to making this moment a reality,” concluded Dr. Owusu. “I am forever grateful to all for your supports!”
ETSU Health Faculty and Students Study Hepatitis C in Rural Appalachia
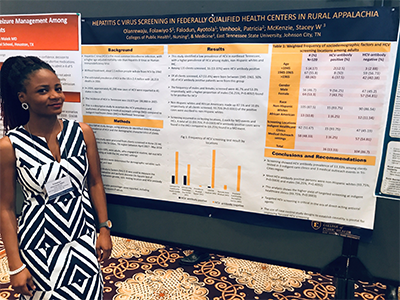
Folawiyo Olanrewaju,
Master of Public Health student, Biostatistics and Epidemiology
Folawiyo Olanrewaju, Master of Public Health student in East Tennessee State University’s College of Public Health, has authored an article in the Healthcare Research and Public Safety Journal. The article, “Hepatitis C Virus Screening In Federally Qualified Health Centers in Rural Appalachia,” is a descriptive study designed to ascertain the Hepatitis C Virus (HCV) prevalence and usefulness of screening in medical outreach settings compared to indigent healthcare clinics in northeast Tennessee. Ms. Olanrewaju recently presented the research at the Southern Regional Meeting of the Southern Society for Clinical Investigations in New Orleans, Louisiana.
Drs. Patricia Vanhook and Stacey McKenzie of the ETSU College of Nursing, along with College of Public Health students Falodun Ayotola, Anthony Peluso, Muhammed Jawla, and Enaholo Omoike are co-authors.
The Hepatitis C Virus (HCV) is a common blood borne infection, with a higher age-adjusted mortality rate than Hepatitis B Virus (HBV) or Human Immunodeficiency Virus (HIV). Recent estimates show that more than 185 million people are infected with HCV worldwide. The prevalence of HCV in the US is estimated at 2.7 to 3.9 cases per 100, 000 with 19 659 deaths in 2014. Without treatment, nearly 1.1 million people will die from HCV by 2060. About 34 000 new cases of Hepatitis C Virus were reported in 41 states in the US in 2015. The incidence of HCV in Tennessee was 13,023 per 100,000.
This descriptive study compares the observed outcome of routine HCV screening in medical outreach settings and indigent healthcare clinics in Northeast Tennessee. Between April 2017 and May 2018, routine, opt-out HCV testing was performed in 3 indigent health care clinics and 3 medical outreach sites in the Tri-Cities region of Tennessee. During screening, demographic information was collected and the de-identified data were analyzed.
A total of 120 persons were screened for HCV. Among these, 16 were HCV-antibody positive. Of all patients screened, 67 (55.8%) were born between 1945 and 1965. 50% of HCV-antibody positive patients were from this group. The frequency of males and females screened were 46.7% and 53.3% respectively, with a higher proportion of males found to be positive for HCV. Screening demonstrated HCV antibody prevalence of 13.33% among clients tested in three indigent care clinics and three medical outreach events the in Tri-Cities region. Most HCV-antibody positive persons were non-Hispanic whites (93.75%) in the indigent care clinics.
The study identified a low prevalence of the Hepatitis C Virus in northeast Tennessee, with a higher prevalence of Hepatitis C Virus among young adults, females, non-Hispanic whites and indigent healthcare clinics. In this era of opioid epidemic contributing significantly to the rates of HCV infection and the availability of direct-acting antiviral agents that over a sustained virologic response rate of more 90%, the benefits of targeted screening cannot be over emphasized.

CPH Alumni and Faculty Publish on Tobacco Use in Middle School Students
Dr. Daniel Owusu
Alumnus, Epidemiology
Dr. Daniel Owusu, alumnus of the Doctor of Public Health program in East Tennessee State University College of Public Health, has authored an article in Substance Use and Misuse. The article, “Intention to Try Tobacco Among Middle School Students in a Predominantly Rural Environment of Central Appalachia” discusses tobacco use rates and associated factors among rural youth.
Drs. Hadii Mamudu, Liang Wang, and Mary Ann Littleton are faculty co-authors. College of Public Health alumni Crystal Robertson Besse and Candice Collins along with undergraduate research assistant Holdon Guy and Nashville State Community College faculty member Rafie Boghozian are additional co-authors.
Tobacco smoking remains the leading preventable cause of morbidity and mortality in the United States. Over 36.5 million people in the U.S. continue to smoke and tobacco use accounts for over 480,000 annual deaths and about $300 billion in economic costs. Tobacco control has become complicated due to the invention and popularity of new tobacco products, including hookah/waterpipe, little cigar and cigarillos (LCCs), and electronic cigarettes (e-cigarettes). In particular, research reports show that e-cigarettes have become the most commonly used tobacco product among youth.
Disparities in tobacco use exist across regions in the United States. The Central Appalachian region carries very high rates of tobacco use prevalence but research on tobacco use initiation is sparse. The objective of this study was to investigate the intention to try tobacco and its associated factors among nonsmoking youth.
Data were obtained from 539 school-based tobacco surveys conducted in 11 middle schools (6th–8th grades; aged 10–15 years) in Northeast Tennessee in 2015–2016. Nonsmoking participants without firm commitment to abstain from trying tobacco in the next year were considered to have an intention to try tobacco. The Full Information Maximum Likelihood estimation (FIML) method in Mplus was employed to conduct a multivariable logistic regression analysis to delineate correlates of intention to try tobacco.
Overall, 20.0% of participants intended to try tobacco. Among participants with the intention to try tobacco, 53.7% owned tobacco-branded item(s), 86.1% believed that tobacco users have more friends, and 88.9% lived with tobacco users. The researchers suggest that individual, interpersonal, and community level factors influence intention to try tobacco in this environment where tobacco pre-emption laws impede development of local tobacco control policies and regulations.
A concerning proportion of the participants intend to try tobacco in the next year. Tobacco promotions and interpersonal factors are significantly associated with the intention to try tobacco. This study provides a baseline for monitoring intention to use tobacco in this high-risk population, and the results suggest the need to implement strong school-based anti-tobacco programs in the midst of tobacco preemption laws that prevent local tobacco policies and regulations.

College of Public Health Faculty and Alumna Publish on Obesity
Dr. Shaoqing Gong
Alumnus, Epidemiology
Shaoqing Gong, 2017 alumna of the East Tennessee State University College of Public Health’s Doctor of Public Health program in Epidemiology, has published on changes in obesity rates among Asian Americans. The article, “The influence of immigrant generation on obesity among Asian Americans in California from 2013 to 2014” was published in the February 2019 edition of PLOS ONE.
Drs. Kesheng Wang and Arsham Alamian, faculty in the Departments of Biostatistics and Epidemiology, and Dr. Ying Li, faculty in the Department of Environmental and Occupational Health and Safety Sciences, are co-authors.
Asian immigrants first came to the United States in significant numbers more than a century and a half ago, mainly as low-skilled male laborers who mined, farmed and built the railroads. In 2014, among a total 42.4 million immigrants in the U.S., Asian Americans accounted for 42.4%. The health of an immigrant population is a function of influences derived from the sending country, the receiving country, and the migration and resettlement experience itself. The existence of a healthy immigrant effect, i.e., that immigrants are on average healthier than the native born, is a widely cited phenomenon across a multitude of literatures including epidemiology and the social sciences. To date, however, there is very limited research examining the influence of immigrant generation on obesity among Asian Americans.
The aim of this research was to analyze the association of immigration generation and obesity among Asian Americans in California. The research team analyzed data from a large population-based sample that is representative of Asian ethnic groups: Chinese, Filipino, Vietnamese, Korean, and Japanese. In contrast, most national surveys on health sample a small number of Asian Americans. Further, they pooled weighted data from the latest cycle of California population, i.e., 2013–2014. The results of this study can help to refine the diverse risk profile for obesity among Asian Americans while also contributing to the overall understanding of the impact of migration on chronic health conditions.
Overall, 23.3% of the Asian population was obese, and 40.0% was overweight. The percentage of 1st, 2nd, and 3rd generation were 72.7%, 22.6%, and 4.6%, respectively. Overall, 1st generation of Asians had lower odds of being obese compared to Whites. Multiple logistic regression analyses showed that overall, 2nd generation and 3rd generation Asians had higher odds of being obese compared to 1st generation Asians. Among Chinese, compared to the 1st generation, the 3rd generation had increased likelihood of being obese.
Compared to Whites, Hispanics, and Blacks, Asian immigrants are less likely to be obese. Among Asians, 2nd and 3rd generations were more likely to be obese than 1st generation. The obesity rate seems to increase the longer Asian immigrants remain in the United States. The results of this study can help to better understand the diverse risk profile for obesity among Asian Americans while also contributing to the overall understanding of the impact of migration on chronic health conditions.

ETSU Study Examines Cardiovascular Risk Factors of Hispanic Children
Dr. Basil Alhassan
Alumnus, Epidemiology
A recent study by researchers at East Tennessee State University sheds new light on the relationship between maternal physical activity and the cardiovascular health of Hispanic children.
Dr. Basil Alhassan, an alumnus of ETSU’s Doctor of Public Health in Epidemiology program, has published an article in PeerJ that discusses the relationship between maternal physical activity and body mass index (BMI) and blood pressure, physical activity and BMI in Hispanic preadolescents.
Drs. Ying Liu, Deborah Slawson, Jonathan Peterson and Arsham Alamian, faculty in the ETSU College of Public Health, are co-authors. Additional co-authors include ETSU faculty members Dr. Jo-Ann Marrs of the College of Nursing and Dr. William A. Clark of the College of Health Sciences.
“Studies have shown physical inactivity, elevated blood pressure, and being overweight or obese track from childhood to adulthood and increase the risk of cardiovascular diseases, such as heart disease and stroke,” Alamian said. “We’ve also seen a correlation between maternal obesity and physical inactivity and obesity and inactivity in older preadolescents.
“However, our study is the first to explore this relationship in Hispanic preadolescents.”
The researchers, led by Alamian, chair of the APPalachian Obesity and METabolic Diseases (APPOMET) Working Group at ETSU, used data collected from 118 Hispanic children enrolled in a metabolic syndrome study in Johnson City.
The investigators determined that about four out of every 10 preadolescents were overweight or obese and about three out of 10 had elevated blood pressure.
This study also found that preadolescents of obese mothers were 6.47 times more likely than preadolescents of mothers with normal BMI to engage in less than three days of at least 60 minutes of vigorous physical activity per week.
Compared to preadolescents whose mothers engaged in moderate physical activity, children whose mothers did not engage in moderate physical activity were 2.92 times more likely to engage in less than three days of physical activity per week and were 2.5 times more likely to have elevated blood pressure.
The prevalence of elevated blood pressure among Hispanic preadolescent subjects, especially in 2- to-5- year-olds (45.7 percent) was higher than estimates from national studies.
“The findings suggest the need for public health interventions that would encourage mothers to increase physical activity and improve weight control as a means for reducing obesity and hypertension in Hispanic preadolescents,” the authors concluded.

Dr. Megan Quinn Leads Summer Student Project in Belize
Dr. Megan Quinn
Associate Professor, Epidemiology
Dr. Megan Quinn is no stranger to leading students in real-world epidemiological training experiences outside the United States. In the past, she has taken groups to Nicaragua for summer projects; however, ongoing political unrest in Nicaragua called for a change in locale for this summer's experiential training. Instead, the group traveled to Punta Gorda, Belize, to partner with Hillside Healthcare International (HHCI). HHCI is a faith inspired, non-profit organization dedicated to providing health care and disease prevention to the people of Southern Belize. In addition, the group offers "cuturally-rich educational rotations for medical, nurse practitioner, physician assistant, pharmacy, physical therapy, and public health students that challenges them to better understand their role in international health care."
While in Belize, students participated in a number of outreach and epidemiological projects among the local population. These included implementing tuberculosis education, creating a diabetes management patient tracking tool and data entry guide, quality improvement projects for the public health depratment, working with mobile clinics, and administering an HIV survey.
Dr. Quinn is an Associate Professor in the Department of Biostatistics and Epidemiology in the College of Public Health where she also serves as the Coordinator for Global Health Initiatives. She manages a number of roles within her department. She also teaches several graduate-level classes, including Infectious Disease Epidemiology. In addition, she is a member of the Center for Excellence in Inflammation, Infectious Disease, and Immunity.

Dr. Maisonet Nogueras Funded to Study Endocrine Disrupting Chemicals
Dr. Mildred Maisonet Nogueras
Assistant Professor, Epidemiology
Dr. Mildred Maisonet Nogueras, Assistant Professor in the Department of Biostatistics and Epidemiology in the East Tennessee State University College of Public Health, has received an R03 grant from the National Institute of Environmental Health Sciences of the National Institutes of Health to study prenatal exposure to endocrine disrupting chemicals and anti-müllerian hormone concentrations in female adolescent study participants.
The reproductive lifespan of the woman is largely determined by factors that regulate the number of follicles laid down during fetal development and their subsequent degeneration rate during adult life. Of concern is a possible role of endocrine disrupting chemicals in dysregulating the number of follicles or in promoting depletion of the follicle pool. Endocrine disrupting chemicals have been detected in human ovarian follicular fluid. In addition, concentrations of certain types of these chemicals detected in cord blood and amniotic fluid from pregnant women suggest human fetal exposure and the possibility of follicular alterations beginning at an early developmental stage.
To date, the literature assessing potential human effects of exposure to environmental endocrine disrupting chemicals on markers of ovarian reserve, such as anti-müllerian hormone, is sparse. The goal of the project is to contribute to current knowledge by conducting secondary analysis of data collected in female adolescents participating in the Avon Longitudinal Study of Parents and Children to assess the association of prenatal exposure to perfluoroalkyl sulfonate and organochlorine pesticides with anti-müllerian hormone concentrations.
Dr. Maisonet Nogueras and her team will also assess temporal changes in hormone concentrations in relation to these exposures. The Avon Longitudinal Study of Parents and Children is a population-based, birth cohort with a long follow-up period and extensive data collection including the assessment of clinical measures in a large subset of participants. Results of the proposed study will address the rather sparse, existing evidence and support the development of new hypothesis.
Ifeoma Ozodiegwu to Present at National Session
 Ifeoma Ozodiegwu will present her research poster, titled “Socioeconomic status and
overweight in low-income countries: A case study of the modifying role of education
on the association between household wealth and overweight in Mozambique,” during
the meeting’s Student Poster Session scheduled to take place later this year. The
session is sponsored by the Delta Omega Honorary Society in Public Health through
the Academic Public Health Caucus. Delta Omega hosts a national student poster session
honoring exceptional student research. Each year the selected students are given the
opportunity to present faculty nominated research at the APHA annual meeting. Participants
are awarded a cash prize and certificate.
Ifeoma Ozodiegwu will present her research poster, titled “Socioeconomic status and
overweight in low-income countries: A case study of the modifying role of education
on the association between household wealth and overweight in Mozambique,” during
the meeting’s Student Poster Session scheduled to take place later this year. The
session is sponsored by the Delta Omega Honorary Society in Public Health through
the Academic Public Health Caucus. Delta Omega hosts a national student poster session
honoring exceptional student research. Each year the selected students are given the
opportunity to present faculty nominated research at the APHA annual meeting. Participants
are awarded a cash prize and certificate.
Ozodiegwu is one of just 29 students selected to present her scholarship and research at the APHA meeting in San Diego.
An international student from Nigeria, Ozodiegwu just completed her third year in the doctor of public health program where she is concentrating in epidemiology in the Department of Biostatistics and Epidemiology. She holds a master of public health degree from ETSU and a bachelor’s degree in applied biochemistry from Enugu State University of Science and Technology in Nigeria.
Earlier this year, Ozodiegwu was awarded the inaugural Sherrod Library Graduate Student Scholarship for Excellence in Research at ETSU. She received the award for her paper addressing the relationship between maternal obesity and neonatal mortality in sub-Saharan Africa.
Spring 2018 Student Awards
The Department of Biostatistics and Epidemiology honored its students at two award ceremonies during April 2018. The first was the Annual ETSU College of Public Student Award Ceremony on April 6, 2018 and the second was the ETSU Graduate School Awards Ceremony on April 18, 2018.
Congratulations to our recipients:

Outstanding MPH Epidemiology Student
Oluyemi Rotimi

Outstanding DrPH Epidemiology Student
Chair's Award for Scholarship
Ruby Yadav
 University Libraries - Sherrod Library Graduate Student Scholarship for Excellence
in Research
University Libraries - Sherrod Library Graduate Student Scholarship for Excellence
in Research
Ifeoma D. Ozodiegwu

Student Affairs Housing and Residence Life Housing GA of the Year
Youssoufou Ouedraogo
Women on Wednesdays' talk: 'Environmental Contamination and Human Health'
Dr. Mildred Maisonet Nogueras
Assistant Professor, Epidemiology
Human exposure to environmental contaminants is common. While studies demonstrate that some people may be at higher risk of exposure than others, everyone is exposed to some degree. East Tennessee State University epidemiologist Dr. Mildred Maisonet will discuss this critical issue in a free public lecture on Wednesday, Jan. 31.
“Environmental Contamination and Human Health: Does It Matter?” is the fifth talk in the 2017-18 “Women on Wednesdays” lecture series sponsored by ETSU’s Women’s Studies Program. It will begin at noon in the presentation room of the Multicultural Center, located on the second level of the D.P. Culp University Center, and a light lunch will be provided.
Maisonet, an assistant professor in ETSU’s College of Public Health, will discuss the current research on environmental contamination and human health. She will highlight how and why some people are more vulnerable than others to environmental health risks and provide useful strategies for minimizing those risks.
Prior to joining ETSU in 2014, Maisonet completed her doctoral degree in epidemiology at the Johns Hopkins Bloomberg School of Public Health. In addition to her work at ETSU and Johns Hopkins, she has worked at the Centers for Disease Control and Prevention, the Rollins School of Public Health in Atlanta and the University of Oulu Faculty of Medicine in Finland. Her research specialties include fetal origin of disease and children’s environmental health.
The “Women on Wednesdays” series is designed to raise awareness about the research, scholarship and community engagement that women at ETSU are doing; to provide a venue where women on campus and in the community can discuss and support each other’s work; and to give students an opportunity to meet faculty who could become mentors for their studies.
For more information, call Dr. Phyllis Thompson, director of ETSU Women’s Studies, at 423-439-4125. For disability accommodations, call the ETSU Office of Disability Services at 423-439-8346.
College of Public Health Faculty, Students, and Alumna Publish in International Journal of Public Health
Dr. Megan Quinn
Assistant Professor, Epidemiology
Dr. Megan Quinn, Assistant Professor for the Department of Biostatistics and Epidemiology in the East Tennessee State University College of Public Health, has published an article in the International Journal of Public Health. As reported in the article, “Methods for understanding childhood trauma: modifying the adverse childhood experiences international questionnaire for cultural competency,” Dr. Quinn and her co-authors, adapted the World Health Organization’s international questionnaire for adverse childhood experiences to be culturally appropriate for a low-resource, underserved community in South Africa
Gabrielle Caldara, Heather Owens, Ifeoma Ozodiegwu, and Elaine Loudermilk, graduate students in the Department of Biostatistics and Epidemiology, along with Dr. Jill Stinson of the Department of Psychology and College of Public Health alumna Kathleen Collins, are co-authors. Project Hope United Kingdom’s Thoughtful Path Program in Munsieville, South Africa was integral to the success of the project.
Adverse childhood experiences research based in the United States demonstrates that traumatic stress in childhood can cause negative physical and mental health outcomes. Many developing countries lack extensive research and comprehensive data on exposure to childhood trauma. The World Health Organization ACE international questionnaire (ACEIQ) highlights multiple types of abuse, neglect, and violence while broadening the definition of traumatic stress to include more globally relevant concerns.
The goal of the research project was to modify the questionnaire to use culturally appropriate questions and terminology for Munsieville, an undeveloped township in South Africa. Without adapting the questionnaire to use culturally appropriate questions and terminology, respondents may not have been able to provide appropriate responses.
After meeting to focus groups to modify the survey, it was given to local stakeholders for review and approval. The pilot study demonstrated that the modified questionnaire provides a comprehensive, and culturally appropriate, measure of childhood trauma, leading to increased community participation during a survey conducted in early 2017.
College of Public Health Faculty Research Diabetes among Veterans
Dr. Ying Liu
Assistant Professor, Epidemiology
Dr. Ying Liu, Assistant Professor in the Department of Biostatistics and Epidemiology in the East Tennessee State University College of Public Health, has published a research brief for the Centers for Disease Control and Prevention regarding diabetes among the United States veteran population. The brief, “Prevalence of and Trends in Diabetes Among Veterans, United States, 2005–2014,” examined data from five cycles of the US National Health and Nutrition Examination Survey.
Drs. Kesheng Wang, Shimin Zheng, and Liang Wang from the Department of Biostatistics and Epidemiology along with Dr. Ying Li of the Department of Environmental and Occupational Health and Safety Sciences in the College of Public Health are co-authors. Sonica Sayam of University of Maryland and Xiaonan Shao of Carnegie Mellon University are additional co-authors.
Diabetes was the seventh leading cause of death in the United States in 2013. Approximately 30.3 million Americans had diabetes, including an estimated 7.2 million who had the disease but had not received a diagnosis. The disease is more prevalent among US veterans, who make up 9% of the civilian US population, than among the general population and affects nearly 25% of US Department of Veterans Affairs patients.
NHANES obtained representative samples from 50 states and the District of Columbia. Veteran status was self-identified through participant household interviews. The number of veterans interviewed ranged from 472 to 685 for each cycle from 2005 through 2012.
The researchers found the prevalence of diabetes in veterans in 2013–2014 was 20.5% and the prevalence of undiagnosed diabetes was 3.4%. Diabetes was most prevalent among veterans aged 65 years or older (27%), among male veterans (22%), among veterans with less than 12 years of education (33.5%) and among veterans with an annual income below the federal poverty line (23.8%). The team concluded that effective prevention and intervention approaches are needed to lower diabetes prevalence among US veterans and ultimately improve their health status.
HealthDay and Endocrine Today featured the team’s research in separate media releases.
Detection of Risk Factors and Trends of Oral Health among U.S.
Dr. Ying Liu
Assistant Professor, Epidemiology
Dr. Ying Liu, Assistant Professor, Department of Biostatistics and Epidemiology was a recent recipient of a grant titled, Detection of Risk Factors and Trends of Oral Health among U.S., from the East Tennessee State University, Research Development Committee. The funds will allow Dr. Liu to secure the NHANES database and support data analysis.
While oral health disparities continue to serve as a major health-related threat for a large number of individuals in the U.S., the available evidence would strongly suggest that problems faced by U.S. veterans in this area are currently among the most severe. The objective in this study is to identify those U.S. veterans at greatest risk for oral health issues. The study will utilize data from the National Health and Nutrition Examination Survey (NHANES). To address the critical needs for oral health in U.S. veterans, the planned specific aims are as follows. Specific Aim #1: Determine temporal changes in the oral health status of U.S. veterans. Specific Aim #2: Identify key risk factors that predict oral health problems in U.S. veterans.
At the completion of this research, Dr. Liu’s expectation is to have identified key risk factors that predict oral health status and temporal changes of oral health status in U.S. veterans. These results can ultimately be expected to have a significant positive impact on development of cost-effective interventions to improve the oral health among U.S. veterans. The successful completion of this project will also provide better targeting of available resources and monitoring of veterans’ oral health status, and aid in developing policies to improve the oral health of U.S. veterans, a too often neglected population.
Drs. Abraham Alhassan and Arsham Alamian Featured in Illuminated: Cardiovascular Health Risks in Hispanic Children
Dr. Abraham Alhassan
DrPH Alumnus, Epidemiology
Dr. Arsham Alamian
Associate Professor, Biostatistics and Epidemiology
Abraham Alhassan, Doctor of Public Health graduate with a concentration in Epidemiology, and Dr. Arsham Alamian, Assistant Professor in the Department of Biostatistics and Epidemiology, have studied the prevalence of cardiovascular risk factors in the investigation of metabolic syndrome among Hispanic children in Johnson City, TN. For his dissertation, Abraham focused on three topics that influence health outcomes: diet, sociodemographic factors and biomarkers to examine their association with cardiovascular diseases among Hispanic children. Abraham graduated Spring 2017 and is pursuing a career in public health practice.
 Stout Drive Road Closure
Stout Drive Road Closure